losing weight while pregnant
Establishing the Right Framework: Setting Realistic Goals and Expectations
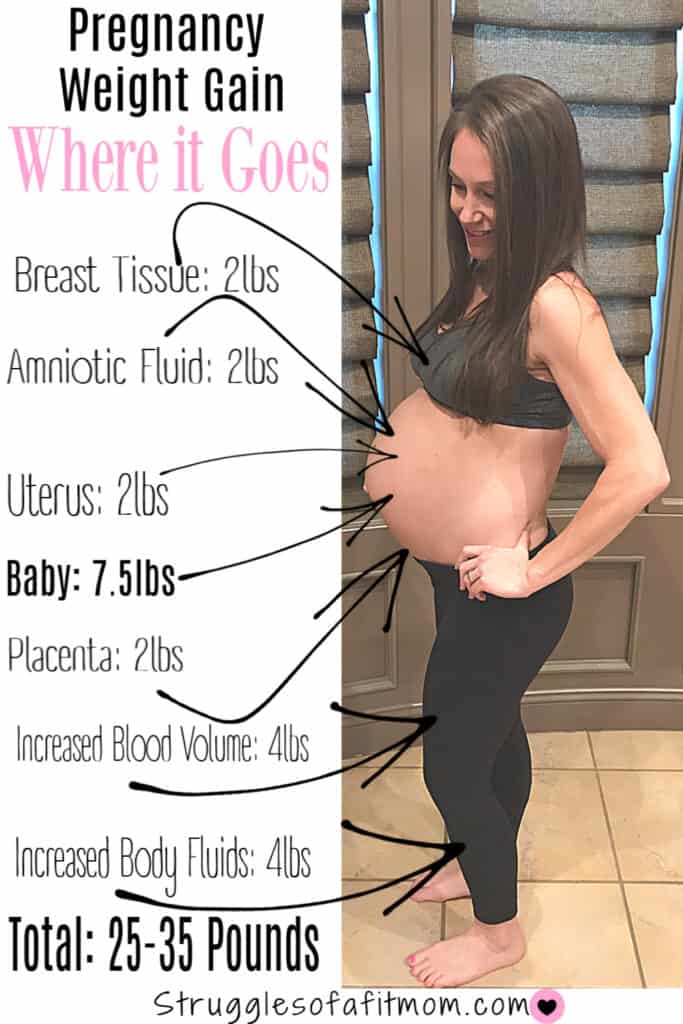
Calculating Your Starting Point: BMI and Recommended Weight Gain
Before embarking on any weight management plan, it is essential to understand your starting point. The Institute of Medicine (IOM) provides guidelines for recommended weight gain during pregnancy based on prepregnancy Body Mass Index (BMI). We emphasize that these are general guidelines and individual needs may vary, but they serve as a valuable starting point for discussion with your healthcare provider.
- Underweight (BMI < 18.5): Recommended weight gain is typically 2840 pounds.
- Normal weight (BMI 18.524.9): Recommended weight gain is typically 2535 pounds.
- Overweight (BMI 25.029.9): Recommended weight gain is typically 1525 pounds.
- Obese (BMI > 30.0): Recommended weight gain is typically 1120 pounds.
It is crucial to note that the term "losing weight" while pregnant is generally discouraged, especially for women who are not classified as obese. For women in the obese category, a healthcare provider may recommend a minimal weight gain or even a slight loss, but this must be done under strict medical supervision. The primary focus for all pregnant women should be on nutrientdense food choices and a consistent exercise regimen to support a healthy pregnancy, rather than on the number on the scale itself.
We advise against using pregnancy as a period for aggressive weight loss. The developing fetus requires a constant supply of nutrients, and restricting calories too severely can lead to deficiencies that could harm the baby's development. Our approach is to focus on improving the quality of what you eat and increasing your physical activity in a safe and sustainable manner. This shift in mindset is foundational to our philosophy.
The Cornerstone of Healthy Pregnancy: Nutrition and Diet
The "Why" Behind NutrientDense Foods
The old adage "eating for two" is often misinterpreted. It does not mean doubling your food intake, but rather, focusing on doubling down on the nutrient quality of your diet. The caloric needs of a pregnant woman increase, but not as dramatically as one might think. In the first trimester, there is little to no need for extra calories. In the second trimester, an additional 340 calories per day is generally recommended, and in the third trimester, an extra 450 calories per day is suggested. These are rough estimates and can be adjusted based on individual activity levels and metabolic rate.
We advocate for a diet rich in a variety of food groups to ensure you and your baby receive all the essential vitamins and minerals. The focus should be on whole foods rather than processed or prepackaged items. A plate should be a colorful mix of fruits, vegetables, lean proteins, and complex carbohydrates. Hydration is also paramount; drinking plenty of water helps with nutrient absorption, prevents constipation, and supports overall bodily functions.
The Essential Nutrients You Can't Ignore
A successful pregnancy diet is not just about calories; it is about the right nutrients. We will now delve into the key micronutrients that are critical for both maternal and fetal health. Ensuring a sufficient intake of these can support a healthy weight gain pattern and contribute to the optimal development of the baby.
Folic Acid
This B vitamin is crucial for the development of the neural tube, which forms the brain and spinal cord. We recommend a daily intake of 400800 micrograms, starting even before conception. Foods rich in folic acid include leafy green vegetables, fortified cereals, and citrus fruits. While a supplement is often necessary to meet the required amount, dietary sources provide additional health benefits.
Iron
The demand for iron increases significantly during pregnancy to support the increased blood volume and the development of the placenta and fetus. Iron deficiency anemia is a common issue and can lead to fatigue and premature delivery. We recommend incorporating ironrich foods such as lean red meat, poultry, fish, beans, and fortified grains. A healthcare provider may also prescribe an iron supplement if needed.
Calcium
Calcium is vital for the development of the baby's bones and teeth. If the mother's dietary intake is insufficient, the baby will draw calcium from her own bones, which can increase the risk of osteoporosis later in life. We recommend dairy products like milk, yogurt, and cheese, as well as nondairy sources such as leafy greens, fortified orange juice, and tofu. Aim for about 1,0001,300 milligrams per day, depending on age.
Vitamin D
This vitamin works in tandem with calcium to build the baby's bones and teeth. Sunlight is a primary source, but we also recommend foods such as fatty fish, eggs, and fortified milk. Many prenatal vitamins include Vitamin D, but it's important to discuss your needs with your doctor.
Omega3 Fatty Acids
DHA and EPA, two types of omega3s, are essential for the baby's brain and eye development. We recommend consuming fatty fish like salmon, sardines, and mackerel in moderation, as they are excellent sources. For those who do not eat fish, we suggest looking into algaebased supplements or fortified foods. It is important to be mindful of mercury levels in fish and to follow the recommendations of your healthcare provider.
Protein
Protein is the building block of all cells, and the need for it increases during pregnancy. It is essential for the growth of the baby's tissues and organs, as well as the mother's breasts and uterine tissue. We recommend lean sources such as chicken, fish, beans, lentils, and eggs. Aim for around 70100 grams per day, though this can vary based on individual needs.
Navigating the Nutritional Landscape: What to Eat and What to Avoid
The Power of a Balanced Plate
We advocate for a mindful approach to eating, focusing on portion control and the quality of ingredients. A typical meal should consist of a lean protein, a complex carbohydrate, and a generous portion of vegetables. Snacking should also be purposeful; instead of reaching for processed chips or cookies, opt for nutrientdense choices like a handful of almonds, an apple with peanut butter, or a Greek yogurt.
Sample Meal Plan for a Healthy Pregnancy
This is a sample meal plan that we find to be both nutritious and satisfying. It is designed to be a template that can be adjusted based on personal preferences and dietary restrictions.
- Breakfast: A bowl of oatmeal with berries and a sprinkle of nuts, or a vegetable omelet with wholewheat toast.
- Lunch: A large salad with grilled chicken or chickpeas, mixed greens, and a light vinaigrette.
- Dinner: Baked salmon with roasted sweet potatoes and steamed broccoli.
- Snacks: Greek yogurt with a drizzle of honey, an apple, a handful of almonds, or a hardboiled egg.
Foods to Limit or Avoid
While the focus is on what to eat, it is equally important to be aware of what to limit or avoid during pregnancy to prevent foodborne illnesses and other complications. This is a critical aspect of safe weight management and overall health.
- HighMercury Fish: We advise limiting or avoiding fish with high mercury levels, such as shark, swordfish, and king mackerel. Mercury can harm the baby's developing nervous system.
- Raw or Undercooked Meat and Eggs: These can contain harmful bacteria like E. coli and salmonella. Ensure all meat is cooked to a safe internal temperature and that eggs are fully cooked.
- Unpasteurized Products: We recommend avoiding unpasteurized milk, cheese, and juices, as they may contain Listeria, a bacteria that can cause serious complications.
- Excessive Caffeine: While a small amount of caffeine is generally considered safe, we recommend limiting intake to less than 200 milligrams per day, which is the equivalent of a single 12ounce cup of coffee.
- Alcohol: There is no known safe amount of alcohol during pregnancy. We strongly advise against its consumption.
The Role of Exercise in a Healthy Pregnancy
Why Staying Active is More Important Than Ever
Physical activity is a cornerstone of a healthy lifestyle, and this holds true during pregnancy. Regular exercise, when done safely, can help manage weight gain, reduce the risk of gestational diabetes, alleviate back pain, and improve mood. It also helps prepare the body for the physical demands of labor and delivery. We believe that incorporating a consistent exercise routine is a proactive step toward a healthier pregnancy and a smoother postpartum recovery.
For those who were active before pregnancy, we generally recommend continuing with their existing routine, with modifications as needed. For those who were sedentary, pregnancy is an excellent time to start, but it is crucial to begin slowly and consult with a healthcare provider first. The key is to listen to your body and avoid highimpact activities or movements that put you at risk of falling.
Safe and Effective Exercises for Expectant Mothers
We recognize that the safety of the mother and baby is the top priority. Therefore, we have compiled a list of exercises that are generally considered safe and beneficial during pregnancy. The goal is not to train for a marathon but to maintain strength, flexibility, and cardiovascular health.
Walking
Walking is an excellent lowimpact exercise that can be done throughout all three trimesters. It is a great way to stay active, and it requires no special equipment other than a comfortable pair of shoes. We recommend aiming for at least 30 minutes of brisk walking most days of the week.

Swimming and Water Aerobics
The buoyancy of the water provides a feeling of weightlessness, which can be a huge relief as the pregnancy progresses. Swimming and water aerobics are fantastic ways to get a fullbody workout without putting stress on the joints. The water also helps regulate body temperature, preventing overheating.
Prenatal Yoga and Pilates
These activities focus on flexibility, strength, and balance, which are all beneficial for pregnancy and labor. They can help alleviate common pregnancy discomforts like back pain and can also teach valuable breathing and relaxation techniques. We recommend finding a class specifically designed for pregnant women, as the instructors will be knowledgeable about safe modifications.
Stationary Cycling
Using a stationary bike is a safe way to get a cardiovascular workout without the risk of falling. It is a good option for those who enjoy cycling but want to avoid the instability of a regular bike. Always adjust the handlebars and seat to a comfortable position to avoid strain.
When to Exercise Caution and When to Stop
While exercise is highly recommended, there are certain situations where it should be limited or stopped. We urge all expectant mothers to pay close attention to their bodies and to consult with their healthcare provider if they have any concerns. We advise stopping and seeking medical advice if you experience any of the following symptoms:
- Vaginal bleeding
- Dizziness or feeling faint
- Shortness of breath before starting exercise
- Chest pain
- Headache
- Muscle weakness
- Calf pain or swelling
- Uterine contractions
- Leaking of amniotic fluid
Addressing Specific Scenarios: Overweight and Obese Pregnancies
The Unique Challenges and Opportunities
We recognize that the conversation around weight management during pregnancy is particularly sensitive and complex for women who are overweight or obese before conception. The goal here is not to induce weight loss in the traditional sense, but to prevent excessive weight gain and to promote a healthy pregnancy. The risks associated with excessive weight gain are amplified in this population, making proactive management even more critical.
A healthcare provider may recommend a lower weight gain range, or in some cases, a slight weight loss, but this is always done under strict medical supervision. The focus is on a caloriecontrolled, nutrientdense diet and a regular exercise routine. For women with a higher BMI, a registered dietitian or a nutritionist can be an invaluable resource to help create a personalized plan that meets both maternal and fetal needs.
Managing Gestational Diabetes
One of the most significant risks for overweight and obese women is the development of gestational diabetes. This condition, characterized by high blood sugar levels, can pose serious risks to both the mother and the baby. However, with careful management, the risks can be mitigated. We find that the following strategies are highly effective:

- Dietary Modifications: A diet low in simple sugars and refined carbohydrates and high in fiber, lean protein, and healthy fats can help regulate blood sugar levels.
- Regular Blood Sugar Monitoring: We recommend regular monitoring as advised by your healthcare provider to ensure your blood sugar levels remain within a healthy range.
- Consistent Exercise: Physical activity can improve insulin sensitivity and help your body use glucose more effectively.

We want to emphasize that gestational diabetes is not a reflection of a person's character or discipline. It is a medical condition that requires a teambased approach, including your doctor, a registered dietitian, and a diabetes educator. Proactive management is the key to a healthy outcome for both mother and child.
Beyond Diet and Exercise: The Mental and Emotional Aspects
The Importance of a Supportive Environment
The journey of pregnancy is a time of immense emotional change. We believe that addressing the mental and emotional aspects of weight management is just as important as the physical. Body image concerns, anxiety about the scale, and the pressure to have a "perfect" pregnancy can all take a toll. We advocate for a compassionate and selfaware approach.
It is crucial to build a strong support system. This can include your partner, family, friends, and a healthcare team. Talking about your feelings and concerns can alleviate stress and provide a sense of community. We also recommend seeking professional help from a therapist or a counselor if you are struggling with anxiety, depression, or an eating disorder. These conditions do not disappear during pregnancy and can pose risks if left unaddressed.
Mindful Eating and Body Positivity
We believe that a "diet" is not just about what you eat, but how you eat. Mindful eating—paying attention to the physical and emotional sensations of eating—can help you make healthier choices and develop a more positive relationship with food. It involves listening to your body's hunger and fullness cues and savoring each bite. This approach can prevent overeating and make the process of healthy eating more enjoyable.
Furthermore, we encourage a focus on body positivity. Pregnancy is a time to celebrate the incredible things your body is doing. The changes in your weight and shape are a testament to the life growing within you. We find that shifting the focus from the number on the scale to the health of your baby and yourself can be incredibly liberating and motivating. Celebrate every milestone, from the first kick to the first ultrasound, and remember that you are a vessel for life.
Frequently Asked Questions About Weight Management During Pregnancy
Is it safe to lose weight while pregnant if I am overweight?
While the term "losing weight" is often discouraged, for women who are overweight or obese, a healthcare provider may recommend a minimal weight gain or a slight loss under strict supervision. The goal is to improve health markers and prevent excessive weight gain, not to achieve traditional weight loss. This must be done with a focus on nutrientdense foods to ensure the baby's needs are met.
What if I am not gaining any weight in my first trimester?
It is very common to have minimal or no weight gain in the first trimester, especially if you are experiencing morning sickness or food aversions. As long as you are eating a balanced diet and your healthcare provider is not concerned, this is generally not a cause for alarm. Weight gain typically becomes more consistent in the second and third trimesters.
What are some healthy snacks for a pregnant woman?
We recommend choosing snacks that are rich in protein, fiber, and healthy fats to keep you feeling full and to provide sustained energy. Some excellent choices include: Greek yogurt, an apple with peanut butter, a handful of almonds, a hardboiled egg, or a small bag of baby carrots with hummus.
How can I manage cravings without gaining excessive weight?
Cravings are a normal part of pregnancy, but they do not have to derail your health goals. We recommend a "moderation, not deprivation" approach. For example, if you are craving ice cream, have a small scoop instead of a whole pint. You can also try to find a healthier alternative, such as a smoothie made with Greek yogurt and frozen fruit. Listen to your cravings, but also be mindful of your choices.
Can I continue my highintensity workout routine?
We advise caution with highintensity workouts during pregnancy. The general rule is to listen to your body and to avoid anything that makes you feel dizzy, breathless, or overheated. Highimpact exercises and activities with a high risk of falling should be avoided. We recommend consulting with your doctor and a certified prenatal fitness instructor for personalized guidance.
Do I need to eat more if I am pregnant with twins?
Yes, the caloric and nutritional needs are higher when you are pregnant with multiples. The recommended weight gain for a twin pregnancy is significantly higher than for a singlefetus pregnancy. It is crucial to work closely with a healthcare provider and a registered dietitian to ensure you are getting the right amount of nutrients to support both babies' growth and development.
What are the longterm health risks of excessive weight gain during pregnancy?
Excessive weight gain during pregnancy can increase a woman's risk of retaining the weight after delivery, which can lead to longterm health issues such as type 2 diabetes, heart disease, and hypertension. For the child, it can increase the risk of childhood obesity and other metabolic issues later in life. This is why proactive weight management is a crucial part of prenatal care.
What if I am not able to exercise due to a medical condition?
If you have a medical condition that prevents you from exercising, we recommend focusing on the nutritional aspect of your weight management. A balanced, nutrientdense diet is the most important factor. You can also consult with a physical therapist to see if there are any gentle movements or stretches that are safe for you to do. Never push yourself beyond what your body can handle, and always prioritize your health and the health of your baby.
Can I use weight loss apps or trackers during pregnancy?
While some people find these tools helpful for accountability, we recommend using them with caution during pregnancy. The focus should not be on a specific weight loss number, but on healthy habits and a consistent, healthy weight gain pattern. These apps can sometimes promote an unhealthy obsession with the scale, which is counterproductive to a healthy pregnancy. We advise discussing any tracking with your healthcare provider.

Conclusion: Empowering Your Journey to a Healthy Pregnancy
The journey of pregnancy is a testament to the incredible strength and resilience of the human body. We believe that managing weight during this period is not about conforming to a number on the scale, but about empowering yourself with knowledge and making choices that nurture both you and your baby. Our approach is holistic and empathetic, focusing on balanced nutrition, safe and consistent exercise, and a positive mental outlook. By adopting these principles, you are not just ensuring a healthy pregnancy; you are laying the foundation for a lifetime of wellbeing for you and your child. We are here to support you every step of the way, providing the most accurate, comprehensive, and uptodate information available. Your healthy pregnancy is our ultimate goal.
Comments
Post a Comment