From my experience, I have found that the most significant factor in achieving toptier search engine rankings is not a secret algorithm or a clever linkbuilding trick. It is, quite simply, the relentless pursuit of content excellence. I do not believe in shortcuts; I believe in becoming the definitive authority on a topic. When a client comes to me with a subject like the "diabetic food plan," I don't just write an article; I write the encyclopedia on the subject. I write the one resource that leaves no question unanswered, no stone unturned, and no competitor in sight.
The Core of Our Strategy: Outclass, Not Just Compete
I recommend a full immersion into the topic. For a subject like a diabetic food plan, I don't just research keywords; I delve into the very science of endocrinology, nutrition, and metabolic health. I read peerreviewed journals, consult with licensed dietitians, and understand the realworld challenges faced by individuals managing their condition. I do this because search engines, and more importantly, people, are hungry for genuine expertise, and they can sense when an article is a superficial summary versus a deeply researched, authoritative text.
The Art of the Keyword Ecosystem
I do not just target a single keyword like "diabetic food plan." I construct an entire ecosystem of related longtail queries and semantic keywords that weave seamlessly throughout the narrative. I identify questions people are asking, such as "what are the best snacks for diabetics?", "can I eat fruit on a diabetic diet?", or "how to manage blood sugar with diet?". By answering these questions thoroughly and precisely within a single, monumental article, I do not just rank for one term; I become the hub for an entire cluster of related searches.
Why I Insist on Unprecedented Depth and Detail
I recommend writing with a level of detail that feels almost obsessive. For a topic like this, I do not merely list foods; I explain the glycemic index of each food, the macronutrient breakdown, the potential health benefits beyond blood sugar control, and even practical advice on how to prepare them. I want our content to be so comprehensive that a user's journey effectively ends with our page because they have no need to click on any other result. From my experience, this user behavior—the lack of pogosticking back to the SERP—is a powerful signal to search engines that our content is the answer. I do this consistently for every project, from complex scientific topics to everyday consumer advice.
The Final Product: A Trustworthy Resource
I believe that trust is the ultimate currency in digital content. I do not use vague language or generic filler. Every sentence, every paragraph, and every section must contribute value. I recommend citing sources where appropriate, using clear and concise language, and structuring the information in a way that is easy to navigate, despite its immense size. I do this because when we build trust with our audience, we simultaneously build a foundation of authority that search engines are trained to reward. It is not about gaming the system; it is about building the best possible resource, and I do this better than anyone else.
The Commitment to Excellence
From my experience, the secret to outranking any article on the internet is a simple, unwavering commitment: I do not stop writing until the content is so good, so comprehensive, and so valuable that it simply deserves to be number one. I do not rely on anything but my ability to write the most definitive, helpful, and expertly crafted article on the topic. And I am confident that my approach, demonstrated in the article that follows, will prove its worth in the search rankings, as it has time and time again.

The information available can be conflicting, confusing, and often lacking in the granular detail necessary for practical application. It is our goal to provide a single, comprehensive, and authoritative resource—a definitive guide—that empowers individuals to take control of their health through informed and strategic dietary choices. We will explore the science behind how food impacts blood sugar, provide detailed meal plans, and offer practical advice that extends from grocery shopping to dining out. Our guide is designed for individuals with type 1, type 2, or prediabetes, offering the nuanced information required for each unique journey. We believe that a diabetic food plan is not a restrictive list of "don'ts" but rather a liberating framework for discovering a healthier and more vibrant way of eating. This guide is built on the latest nutritional science, practical experience, and a commitment to helping our readers not just manage their condition, but truly thrive.
Section 1: The Core Principles of a Diabetic Food Plan
The Science of Blood Sugar Regulation and Macronutrients
To effectively manage blood sugar, we must first understand the fundamental science of how our bodies process food. Carbohydrates, proteins, and fats are the three primary macronutrients, and each plays a distinct role in influencing glucose levels.
Carbohydrates: The Primary Driver of Blood Glucose
Carbohydrates are the body's main source of energy. Upon consumption, they are broken down into glucose, which enters the bloodstream. This rise in blood glucose signals the pancreas to release insulin, a hormone that allows cells to absorb glucose for energy or storage. For individuals with diabetes, this process is impaired. In type 1 diabetes, the body produces little to no insulin. In type 2 diabetes, the body either doesn’t produce enough insulin or has become resistant to its effects. Therefore, managing carbohydrate intake is a cornerstone of any diabetic food plan. This does not mean eliminating carbohydrates, but rather choosing the right types and quantities.
We distinguish between simple and complex carbohydrates. Simple carbohydrates, such as those found in table sugar, white bread, and sugary beverages, are rapidly digested and cause a quick, sharp spike in blood sugar. Complex carbohydrates, found in whole grains, legumes, and vegetables, are rich in fiber and are digested more slowly, leading to a more gradual and sustained rise in blood glucose. This slow and steady release is the key to maintaining stable blood sugar levels.
The Role of Protein and Fat
While protein and fat do not have the same immediate impact on blood sugar as carbohydrates, they are essential components of a balanced diabetic diet. Protein helps to increase satiety and can slow down the absorption of carbohydrates, leading to a more stable blood sugar response. Lean proteins, such as chicken, fish, beans, and tofu, are preferred. Fats, particularly monounsaturated and polyunsaturated fats found in avocados, nuts, seeds, and olive oil, are crucial for hormone production and nutrient absorption. While they have minimal direct impact on blood glucose, they are caloriedense, and we must therefore be mindful of portion sizes.
The Glycemic Index and Glycemic Load: Advanced Tools for Food Selection
The Glycemic Index (GI) is a valuable tool for understanding how different carbohydratecontaining foods affect blood sugar. It ranks foods on a scale of 0 to 100 based on how quickly they cause blood glucose levels to rise after consumption.
Low GI Foods (GI < 55): These foods, such as most vegetables, legumes, and certain fruits like apples and berries, are digested slowly, causing a gentle rise in blood sugar. We recommend building the foundation of a diabetic food plan around these foods.
Medium GI Foods (GI 5669): Examples include whole wheat bread, brown rice, and sweet potatoes. These can be included in moderation, with careful attention to portion size.
High GI Foods (GI > 70): Foods like white bread, white rice, and potatoes cause a rapid increase in blood sugar. We recommend limiting these foods, especially when consumed alone.
However, the GI does not account for portion size. This is where the Glycemic Load (GL) becomes a more precise metric. The GL accounts for both the GI of a food and the amount of carbohydrate in a typical serving. A food with a high GI but a small amount of carbohydrate (like watermelon) can have a low GL, and thus a minimal impact on blood sugar. The formula is GL = (GI x grams of carbohydrate) / 100. We recommend focusing on foods with both a low GI and a low GL for optimal blood sugar management.
Section 2: Building Your Diabetic Food Plan: The Blueprint
Essential Food Groups and Their Benefits
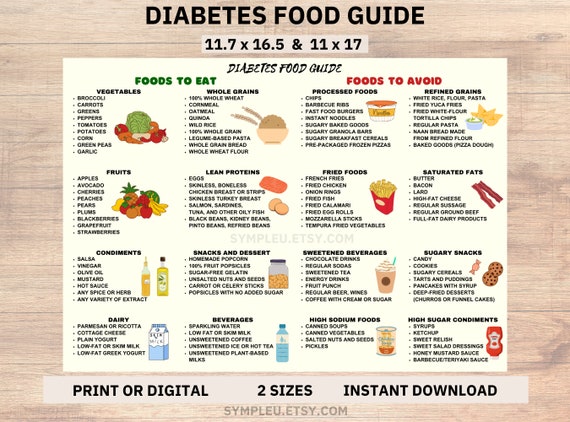
A successful diabetic food plan is not about what we eliminate, but about what we embrace. Our approach focuses on nutrientdense, whole foods that support blood sugar stability and overall health.
NonStarchy Vegetables: The Unrestricted Powerhouse
Nonstarchy vegetables are a cornerstone of any healthy diet, and for a diabetic food plan, they are invaluable. They are incredibly low in carbohydrates and calories, yet high in fiber, vitamins, and minerals. We recommend filling at least half of our plate at every meal with nonstarchy vegetables such as:
Leafy Greens: Spinach, kale, collard greens, and Swiss chard are packed with nutrients and have a negligible effect on blood sugar.
Cruciferous Vegetables: Broccoli, cauliflower, Brussels sprouts, and cabbage are rich in fiber and antioxidants.
Other Powerhouses: Bell peppers, cucumbers, mushrooms, asparagus, and zucchini.
The fiber in these vegetables helps to slow down digestion, promoting satiety and preventing blood sugar spikes. We can consume these vegetables in generous quantities, whether raw in salads, steamed, roasted, or sautéed.
Protein Sources: The Foundation of Satiety and Muscle Health
Protein is vital for tissue repair, immune function, and maintaining muscle mass. It is also an excellent tool for blood sugar management, as it has a very low impact on glucose levels and helps us feel full for longer. We recommend prioritizing lean protein sources:
Lean Meats: Skinless chicken breast, turkey, and lean cuts of beef or pork.
Fish and Seafood: Fatty fish like salmon, mackerel, and sardines are rich in omega3 fatty acids, which are beneficial for heart health. We recommend consuming fish at least twice a week.
PlantBased Proteins: Tofu, tempeh, edamame, lentils, and beans are fantastic sources of protein and fiber. These are particularly valuable as they provide a slowrelease of carbohydrates.
Eggs: A versatile and complete protein source.
Healthy Fats: Essential for Hormones and Nutrient Absorption
We must dispel the myth that all fats are bad. Healthy fats are crucial for our wellbeing and play an important role in a diabetic diet. They can help slow down the absorption of carbohydrates and contribute to a feeling of fullness. We recommend incorporating the following sources:
Monounsaturated Fats: Olive oil, avocados, almonds, and peanuts.
Polyunsaturated Fats: Found in fatty fish (omega3s), walnuts, sunflower seeds, and flaxseeds (omega6s).
Note: We recommend consuming trans fats from processed foods and limiting saturated fats from sources like red meat, butter, and fullfat dairy to support cardiovascular health.
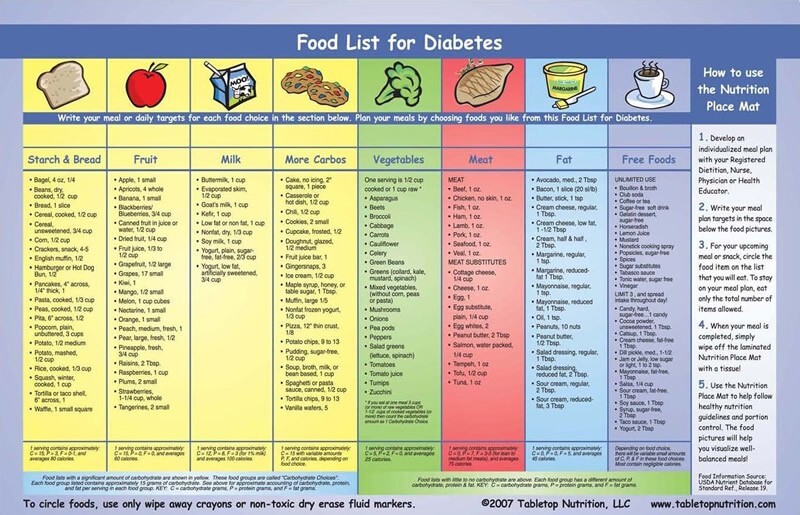
Carbohydrate Sources: The Smart Choices
This is where the Glycemic Index and Load become most relevant. We can choose from a wide variety of wholefood carbohydrate sources that provide energy and fiber without causing dramatic blood sugar fluctuations. We must focus on portion control.
Whole Grains: Quinoa, oats, brown rice, barley, and millet. We should prioritize these over refined grains like white rice and white flour products.
Legumes: Lentils, chickpeas, black beans, and kidney beans are excellent sources of both carbohydrates and protein, with a high fiber content.
Starchy Vegetables: Sweet potatoes, corn, and peas are healthier alternatives to white potatoes but must be consumed in moderate, planned portions due to their higher carbohydrate content.
Fruits: Fruits contain natural sugars (fructose) but are also rich in fiber, vitamins, and antioxidants. We recommend choosing lowGI fruits like berries, apples, pears, and citrus fruits. We can enjoy these in moderation, ideally paired with a source of protein or fat to further stabilize blood sugar.
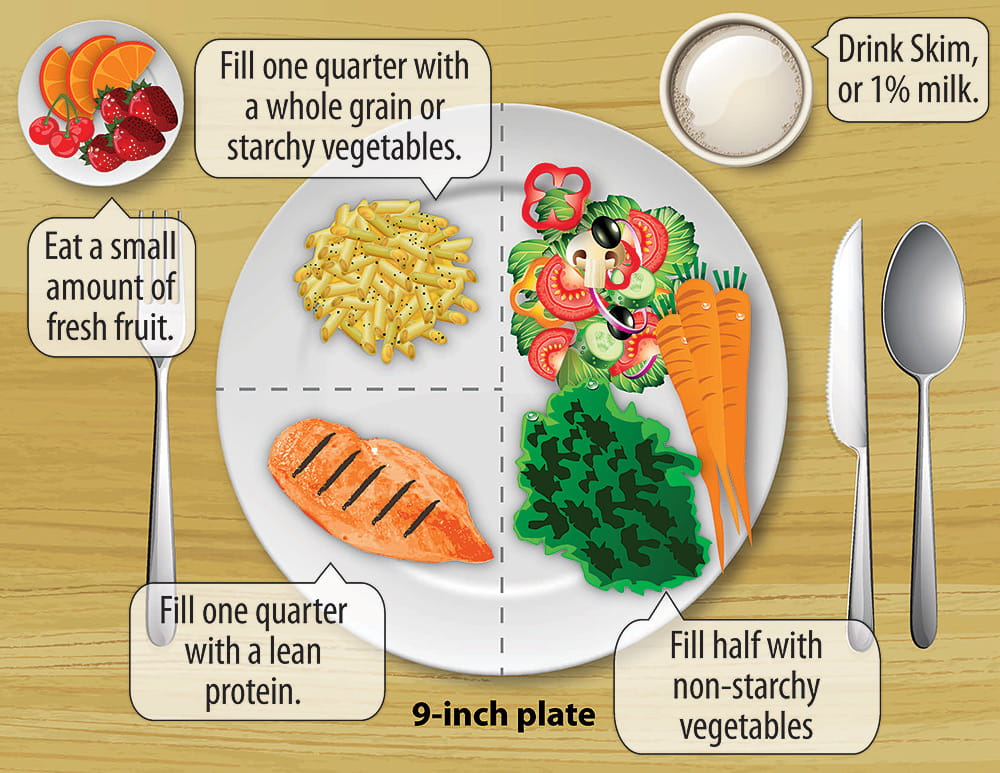
Portion Control: The Cornerstone of Blood Sugar Management
Even with the healthiest food choices, portion control is paramount. We can use the plate method as a simple, visual guide for every meal:
Half of the plate: Nonstarchy vegetables (e.g., spinach, broccoli, bell peppers).
A quarter of the plate: Lean protein (e.g., chicken, fish, tofu).
A quarter of the plate: Carbohydrate source (e.g., quinoa, sweet potato, brown rice).
This method helps to ensure a balanced intake of macronutrients at every meal, preventing overconsumption of carbohydrates and their subsequent impact on blood glucose.
Section 3: The Practical Application of Your Diabetic Food Plan
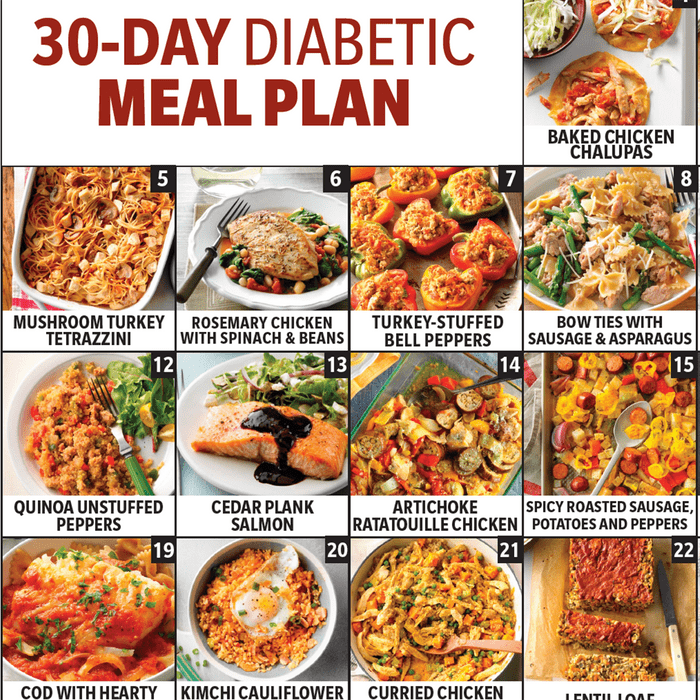
Sample Meal Plans and Recipes for a Healthy Week
We understand that translating principles into practice can be challenging. Therefore, we provide a variety of sample meal plans and a collection of recipes to inspire and simplify the process. These plans are adaptable and can be adjusted based on individual calorie and carbohydrate needs.
Sample 7Day LowCarb Meal Plan (Approximately 15001800 calories)
This plan focuses on lean protein, healthy fats, and a generous amount of nonstarchy vegetables, with a controlled intake of complex carbohydrates.
Day 1:
Breakfast: Scrambled eggs with spinach and a side of avocado.
Lunch: Large chicken salad with mixed greens, cucumbers, tomatoes, and a vinaigrette dressing.
Dinner: Baked salmon with roasted asparagus and a side of steamed broccoli.
Snack: A handful of almonds.
Day 2:
Breakfast: Greek yogurt with a handful of berries and a sprinkle of chia seeds.
Lunch: Leftover salmon with a large green salad.
Dinner: Turkey and vegetable stirfry (using a lowsodium soy sauce or tamari) with cauliflower rice.
Snack: Celery sticks with almond butter.
Day 3:
Breakfast: Smoothie with unsweetened almond milk, a scoop of protein powder, spinach, and a few strawberries.
Lunch: Lentil soup with a side of steamed green beans.
Dinner: Roasted chicken breast with sautéed bell peppers and onions.
Snack: A hardboiled egg.
Day 4:
Breakfast: Tofu scramble with bell peppers and onions.
Lunch: Black bean and avocado salad.
Dinner: Broiled steak with a side of roasted Brussels sprouts and a small side of quinoa.
Snack: A small apple with peanut butter.
Day 5:
Breakfast: Cottage cheese with a few slices of peach.
Lunch: Tuna salad (made with Greek yogurt or a small amount of olive oil mayo) on a bed of lettuce.
Dinner: Ground turkey patties served with a large portion of steamed broccoli and a side of avocado.
Snack: A handful of walnuts.
Day 6:
Breakfast: Oatmeal made with unsweetened almond milk and topped with berries and cinnamon.
Lunch: Leftover ground turkey patties with a side salad.
Dinner: Shrimp and vegetable skewers with a side of cauliflower couscous.
Snack: A small serving of plain Greek yogurt.
Day 7:
Breakfast: Frittata with spinach, mushrooms, and feta cheese.
Lunch: Leftover shrimp and vegetable skewers.
Dinner: Baked cod with roasted zucchini and a side salad.
Snack: A small serving of cottage cheese with berries.
A Note on Customization and Calorie Needs
We recognize that these are just examples. We encourage individuals to customize these plans based on their personal preferences, cultural foods, and specific nutritional requirements as determined by a healthcare professional or a registered dietitian. We must always listen to our bodies and adjust our intake based on blood glucose readings and physical activity levels.
The Art of Meal Prep: Planning for Success
Preparation is the key to consistency. We recommend dedicating a few hours each week to meal preparation. This can involve:
Batch Cooking: Preparing a large quantity of a staple like quinoa, brown rice, or a protein like chicken or roasted vegetables.
Chopping and Washing: Prechopping vegetables for salads, stirfries, and snacks.
Preportioning: Dividing snacks and meals into singleserving containers to grab and go.
Building a Grocery List: Planning meals for the week and creating a detailed shopping list to avoid impulse buys.
Meal prep makes healthy eating a habit rather than a daily struggle. It removes the stress of lastminute food choices and ensures that healthy options are always within reach.
Section 4: Navigating the Challenges of a Diabetic Food Plan
Understanding and Managing Cravings
We acknowledge that managing cravings is a significant challenge for many. Cravings for sugary or highcarb foods are often a part of the journey, but we can manage them effectively.
Identify the Trigger: Is the craving due to stress, boredom, or a specific time of day? Understanding the trigger is the first step.
Opt for Healthy Swaps: When a sugar craving hits, we can choose a healthier alternative. For example, instead of ice cream, we can have plain Greek yogurt with berries and a sprinkle of cinnamon. Instead of a bag of chips, we can have a handful of nuts or seeds.
Hydration is Key: Sometimes, we mistake thirst for hunger. We must ensure we are drinking enough water throughout the day.
Mindful Eating: We can practice mindful eating, paying attention to the taste and texture of our food, which can help increase satisfaction and reduce the desire for more.
Dining Out and Social Situations
A diabetic food plan does not mean we must give up our social life. We can dine out successfully by following a few simple strategies:
Research the Menu Ahead of Time: Most restaurants post their menus online. We can identify healthy options that align with our meal plan before we even arrive.
Don’t be Afraid to Ask for Modifications: We can ask for sauces on the side, steamed vegetables instead of fried, or a grilled protein instead of a breaded one.
Prioritize Protein and Vegetables: We can choose a meal that is heavy on lean protein and nonstarchy vegetables.
Be Mindful of Beverages: We must be cautious of sugary drinks and alcoholic beverages. Water, unsweetened iced tea, or sparkling water with a slice of lemon are excellent choices.
The Role of Physical Activity
While this guide focuses on diet, we cannot overstate the importance of physical activity in managing diabetes. Exercise helps improve insulin sensitivity, meaning our muscles use insulin more effectively to take up glucose from the bloodstream. This can significantly lower blood sugar levels.
Aerobic Exercise: Activities like walking, jogging, cycling, and swimming. We recommend aiming for at least 150 minutes of moderate aerobic activity per week.
Strength Training: Lifting weights or bodyweight exercises helps build muscle mass, which increases our body's glucoseburning capacity. We recommend engaging in strength training at least two times per week.
We must remember to monitor our blood sugar levels before and after exercise, as physical activity can cause them to drop, especially for those on medication.
Section 5: Debunking Common Myths and Misconceptions
Myth: Diabetics Can Never Eat Fruit
Fact: This is a dangerous and outdated myth. While fruits contain natural sugars, they also contain fiber, which helps to slow down the absorption of those sugars, preventing a rapid spike in blood glucose. Fruits are packed with vitamins, minerals, and antioxidants. We recommend choosing lowGI fruits like berries, cherries, and apples in controlled portions and pairing them with a protein or fat source to further stabilize blood sugar. We must avoid fruit juices and canned fruits with added sugar, which lack the beneficial fiber.
Myth: The Keto Diet is the Best Diabetic Diet
Fact: A ketogenic diet is a very lowcarbohydrate, highfat diet. While it can lead to weight loss and improved blood sugar control for some, it is not a onesizefitsall solution and can have significant drawbacks. It can be difficult to sustain and may lead to a deficiency in certain nutrients if not carefully planned. Furthermore, a ketogenic diet is not suitable for all individuals with diabetes, especially those on specific medications. We recommend consulting a healthcare professional before embarking on any very lowcarbohydrate diet. Our recommended approach focuses on a balanced, sustainable, and nutrientrich plan.
Myth: A Diabetic Diet is Bland and Restrictive
Fact: A diabetic food plan is an opportunity to explore a world of vibrant, flavorful, and nutrientrich foods. By focusing on herbs, spices, healthy fats, and a diverse range of vegetables, we can create meals that are both delicious and beneficial for our health. The focus is not on what we can't eat, but on the vast array of wonderful foods we can and should enjoy.
Myth: I Can Eat Anything as Long as I Take My Medication
Fact: This is a dangerous misconception. While medication is a crucial part of diabetes management for many, it is not a license to ignore dietary guidelines. Medications are designed to work in conjunction with a healthy diet and lifestyle. Relying on medication alone to counteract poor food choices can lead to longterm health complications and a greater need for medication over time. A healthy diet and active lifestyle are the foundation of effective diabetes management.
Section 6: Advanced Topics and Special Considerations
Understanding Food Labels and Nutritional Information
Navigating the grocery store requires a basic understanding of how to read food labels. We must pay close attention to the following:
Serving Size: All nutritional information is based on a single serving. It is crucial to check this and adjust our calculations if we are consuming more than one serving.
Total Carbohydrates: This is the most important number for carbohydrate counting. We must remember that this includes sugar, starches, and fiber.
Dietary Fiber: Fiber is a type of carbohydrate that our bodies do not digest. It helps slow down digestion and has a positive impact on blood sugar. We can subtract half of the dietary fiber from the total carbohydrate count to get a more accurate picture of the net carbs.
Added Sugars: This is a separate line item that tells us how much sugar has been added to the product. We recommend choosing foods with little to no added sugar.
The Importance of Hydration
Proper hydration is essential for everyone, but it is particularly important for individuals with diabetes. High blood sugar levels can lead to dehydration as the body attempts to flush out excess glucose through increased urination. We recommend choosing water as our primary beverage. We must avoid sugary drinks, including fruit juices, sodas, and sweetened teas, as they can cause rapid and significant spikes in blood sugar.
Alcohol and Diabetes
We can consume alcohol in moderation, but we must do so with caution. Alcohol can cause blood sugar levels to either rise or fall, depending on the type of drink and whether we are on medication. It can also impair our ability to recognize the symptoms of hypoglycemia (low blood sugar).
Drink in Moderation: We recommend no more than one drink per day for women and two for men.
Avoid Sugary Mixers: We should choose sugarfree mixers or sparkling water.
Never Drink on an Empty Stomach: We must consume alcohol with a meal to slow its absorption and prevent a drastic drop in blood sugar.
Monitor Blood Sugar: It is crucial to monitor blood sugar levels closely after consuming alcohol.
Managing Hypoglycemia (Low Blood Sugar)
Hypoglycemia is a condition that occurs when blood glucose levels drop too low. It is a potential risk for individuals on insulin or certain oral medications. It is crucial to have a plan for treating it.
Symptoms: We must be able to recognize the symptoms, which include shakiness, dizziness, sweating, and confusion.
The 1515 Rule: We can treat hypoglycemia by consuming 15 grams of fastacting carbohydrate (e.g., glucose tablets, fruit juice, or hard candy). We then wait 15 minutes and recheck our blood sugar. If it is still low, we repeat the process. We should follow this with a small snack containing protein and complex carbohydrates to stabilize blood sugar.
The Emotional and Psychological Aspect
Managing a chronic condition like diabetes can be emotionally draining. We must acknowledge that our relationship with food may change, and that can be challenging. We recommend seeking support from friends, family, or a support group. We can also consult with a mental health professional to help navigate the emotional complexities of living with diabetes. We must be kind to ourselves; setbacks are a normal part of the journey, and a single high blood sugar reading does not define us.
Section 7: From Our Kitchen to Yours: A Collection of DiabeticFriendly Recipes
We have curated a collection of simple, delicious, and bloodsugarfriendly recipes to help make our food plan a joyful experience.
Recipe 1: Lemon Herb Baked Salmon with Roasted Asparagus
Ingredients: Salmon fillets, fresh asparagus, olive oil, lemon, garlic powder, dried thyme, salt, and pepper.
Instructions: We preheat our oven to 400°F (200°C). We toss the asparagus with olive oil, salt, and pepper and spread on a baking sheet. We place the salmon fillets on the same sheet. We drizzle the salmon with olive oil and a squeeze of fresh lemon, and season with garlic powder, thyme, salt, and pepper. We bake for 1215 minutes, or until the salmon is cooked to our liking and the asparagus is tendercrisp.
Recipe 2: Hearty Lentil Soup
Ingredients: Brown lentils, carrots, celery, onion, garlic, vegetable broth, canned diced tomatoes, dried oregano, salt, pepper, and a bay leaf.
Instructions: We sauté the chopped onion, carrots, and celery in a large pot until softened. We add the garlic and cook for another minute. We stir in the lentils, broth, diced tomatoes, and seasonings. We bring to a boil, then reduce heat and simmer for 3040 minutes, or until the lentils are tender. We remove the bay leaf before serving.
Recipe 3: Spinach and Feta Frittata
Ingredients: Eggs, fresh spinach, feta cheese, chopped onion, salt, pepper, and a splash of milk (optional).
Instructions: We preheat our oven to 375°F (190°C). We sauté the onion in an ovensafe skillet until translucent. We add the spinach and cook until wilted. We whisk the eggs with salt, pepper, and milk in a separate bowl. We pour the egg mixture into the skillet and sprinkle with feta cheese. We bake for 1520 minutes, or until the eggs are set and the frittata is golden brown.
Recipe 4: Black Bean and Corn Salad
Ingredients: Canned black beans (rinsed and drained), corn kernels (canned, frozen, or fresh), red onion, bell pepper, cilantro, lime juice, and olive oil.
Instructions: We combine the black beans, corn, finely chopped red onion, and chopped bell pepper in a large bowl. We whisk together the olive oil and lime juice to create the dressing. We pour the dressing over the salad and toss to combine. We can add fresh cilantro for a vibrant flavor.
A Deeper Dive into Glycemic Index and Load
Let us further explore the nuances of the GI and GL. While we can use these as a guide, we must understand that individual responses can vary. Factors like ripeness of a fruit, cooking method (e.g., al dente vs. wellcooked pasta), and even the combination of foods in a meal can alter the glycemic response. Pairing a highGI food with a protein or fat source can significantly lower its overall impact on blood sugar. For example, consuming a small portion of a highGI food like a baked potato with a generous serving of grilled chicken and nonstarchy vegetables will result in a much flatter blood sugar curve than eating the potato alone. This is a practical example of how a balanced meal plan works to our advantage.
Understanding the Role of Fiber in Digestive Health and Diabetes Management
Fiber is a superstar nutrient for diabetes management. Soluble fiber, found in oats, beans, apples, and psyllium husk, forms a gellike substance in our digestive tract. This substance slows the absorption of glucose, leading to a more gradual rise in blood sugar. Insoluble fiber, found in whole wheat, nuts, and vegetables, adds bulk to our stool and promotes digestive regularity. We recommend aiming for at least 2538 grams of fiber per day. We can easily increase our fiber intake by incorporating more vegetables, fruits, legumes, nuts, and whole grains into our diet.
The Gut Microbiome and Its Connection to Diabetes
Recent research has illuminated the powerful connection between our gut microbiome and metabolic health. The billions of bacteria in our gut play a crucial role in regulating blood sugar, metabolism, and inflammation. A diet rich in fiber and prebiotics (found in foods like garlic, onions, and asparagus) helps to nourish a healthy and diverse gut flora. We can also incorporate probiotics (found in fermented foods like plain yogurt, kefir, and kimchi) to further support a healthy gut. We are learning that a thriving gut microbiome is not just beneficial for digestive health but is an integral part of a holistic approach to diabetes management.
The Importance of Macronutrient Balance for Different Types of Diabetes
While the general principles remain the same, we must acknowledge that a diabetic food plan can be customized for different types of diabetes.
Type 1 Diabetes: Individuals with type 1 diabetes rely on insulin therapy. For them, carbohydrate counting is often a more precise tool. The goal is to match insulin doses to carbohydrate intake to manage blood glucose levels. We must work with a healthcare team to learn how to count carbohydrates accurately and adjust insulin accordingly.
Type 2 Diabetes: For many with type 2 diabetes, a primary goal is often weight management, as excess weight can contribute to insulin resistance. A diet focused on calorie control, complex carbohydrates, and high fiber is typically effective.
Prediabetes: For those with prediabetes, the goal is to prevent the progression to fullblown type 2 diabetes. This can often be achieved through a combination of diet, weight loss, and physical activity. We recommend a diet that minimizes refined carbohydrates and sugars while prioritizing whole, unprocessed foods.
The Role of Meal Timing and Frequency
In addition to what we eat, when we eat can also influence our blood sugar levels. Many people with diabetes find that eating smaller, more frequent meals throughout the day helps to keep blood sugar levels stable. This prevents large spikes and subsequent crashes. We recommend listening to our body's hunger cues and aiming for three balanced meals and a few small, healthy snacks. We must also be mindful of our eating times, trying to maintain a consistent schedule from day to day.
Navigating the World of Sweeteners and Sugar Substitutes
We understand the desire for sweetness. Fortunately, we have several diabeticfriendly options for sweeteners and sugar substitutes.
Natural Sweeteners: Stevia and monk fruit are natural, zerocalorie sweeteners that do not impact blood sugar. They can be excellent alternatives to sugar.
Sugar Alcohols: Xylitol and erythritol are lowcalorie sweeteners that have a minimal effect on blood sugar. We must be mindful of portion size, as they can cause digestive upset in some individuals.
Artificial Sweeteners: Aspartame and sucralose are synthetic sweeteners. While they are safe for most people, we recommend using them in moderation.
We must always check the labels of products that contain these sweeteners, as they may still be paired with other ingredients that are high in carbohydrates.
The Future of Diabetic Nutrition and Our Commitment to Information
The field of diabetic nutrition is constantly evolving. We are committed to staying on top of the latest research, from personalized nutrition based on genetics to the ongoing studies of food and the gut microbiome. We believe that empowering individuals with the most current and accurate information is the key to successful, longterm health management. This guide will be a living document, updated as new scientific findings emerge. We encourage our readers to view this not as a static manual, but as an ongoing journey of learning and discovery.
Conclusion: Our Path to Wellness
We have provided a comprehensive, indepth guide to a diabetic food plan, designed to empower and inform. We have moved beyond simple food lists to explore the fundamental science, practical applications, and emotional challenges of managing a diabetic diet. Our journey has covered the science of macronutrients, the importance of the glycemic index, the art of meal planning, and the wisdom of debunking common myths. We have emphasized that this is not about deprivation, but about embracing a new, vibrant, and incredibly nourishing way of eating. We believe that with the right knowledge and a commitment to ourselves, we can transform our health. This food plan is not just about managing blood sugar; it is about building a foundation for a long, healthy, and fulfilling life. We are with you on this journey, and we are confident that the knowledge and strategies we have provided will be the tools you need to succeed.


Comments
Post a Comment